Everything About Clean Claims in Medical Billing – Get Paid Faster
You’ve probably heard the phrase “clean claim” thrown around in medical billing. But what is a clean claim, and why does it matter? A clean claim is a claim that gets accepted by the insurance company without any issues. It’s free of errors, missing information, or coding mistakes, which means it doesn’t get rejected or denied. Getting those clean claims through the system smoothly is super important for healthcare providers because it speeds up the payment process and reduces headaches along the way. Let’s break it down further because this process can greatly impact how smoothly things run financially for hospitals and clinics.
What Is a Clean Claim?
A clean claim is simply one with everything correct from the start. It includes accurate patient details, the right medical codes, and all the necessary documentation. No errors, no missing info – it’s ready to go straight through without problems.
Clean Claim VS Rejected or Denied Claim
Now, let’s talk about the difference between a clean claim and one that gets rejected or denied. A clean claim is good to go from the start, while a rejected or denied claim has issues. A rejected claim might be missing some info or have errors that need fixing before resubmitting. On the other hand, a denied claim is one the insurance won’t pay because it doesn’t meet certain coverage rules. So, clean claims are like gold in the billing world—they help avoid all those back-and-forth hassles.
Submitting clean claims is super important for healthcare providers. Why? Because it saves time and reduces delays in getting paid. Clean claims mean fewer rejections, faster payments, and less time wasted on fixing errors.
Importance of Clean Claims in Medical Billing
In medical billing, clean claims are like the fuel that keeps the revenue engine running smoothly. They make sure that payments come in on time, without being stuck in a pile of rejected claims that need fixing. For hospitals and clinics, this means steady cash flow, which is super important for covering expenses and keeping the lights on.
One of the biggest headaches in billing is having claims denied or delayed. Think of a clean claim in medical billing as the fast pass—everything is accurate, so it moves through the system quickly. When claims aren’t clean, they can sit in limbo for days or even weeks, waiting to be corrected. This slows down payments and can mess up cash flow. Clean claims minimize these issues and keep everything moving smoothly.
Impact of Clean Claims on Insurance Processing
Insurance companies also prefer clean claims because they make their job easier. A clean claim in medical billing processes is faster, so it takes less time for them to approve it. In other words, the cleaner the claim, the faster everyone gets paid. It’s a win-win for both the healthcare provider and the insurance company. Plus, fewer errors mean less back-and-forth, saving time for everyone.
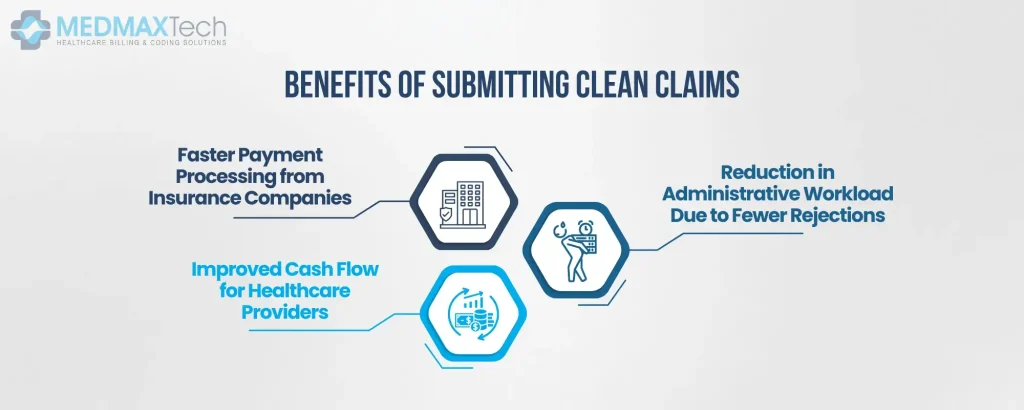
Benefits of Submitting Clean Claims
Submitting clean claims offers a whole lot of benefits, not just for healthcare providers but for everyone involved in the process.
Faster Payment Processing from Insurance Companies
One of the biggest perks of submitting a clean claim in medical billing is faster payment. Insurance companies love when claims are submitted without errors because they can process them quickly. In fact, clean claims are often processed within just a few weeks, whereas rejected or denied claims can take months to resolve. Imagine sending out a perfect invoice and getting paid right away—that’s what clean claims do for hospitals and clinics.
Reduction in Administrative Workload Due to Fewer Rejections
Nobody wants to spend their time fixing mistakes, right? Submitting clean claims saves billers from having to go back and forth with insurance companies. When claims are clean, there’s no need for extra paperwork or follow-ups, which means less stress for your billing team. In some healthcare facilities, up to 65% of rejected claims are due to small errors that could have been avoided. By getting the claim right the first time, you cut down on extra admin work and improve efficiency.
Improved Cash Flow for Healthcare Providers
The faster claims get processed, the quicker the cash flows in. Submitting a clean claim in medical billing ensures that healthcare providers are paid without unnecessary delays. This keeps their operations running smoothly and helps them focus more on patient care, instead of worrying about when they’ll receive payments. According to a study, the average time it takes for a clean claim to be paid is 14 days, whereas claims with errors can take up to 90 days to process
Common Reasons for Claims Rejections
So, what stops a claim from being “clean”? Mistakes can happen at any stage of the billing process, and even the smallest error can lead to rejections. But knowing these common issues helps reduce errors and ensures more clean claims get submitted.
One of the top reasons a claim isn’t considered clean is inaccurate patient information. Think of things like wrong policy numbers or missing addresses. Other common issues include incorrect coding, duplicate claims, or incomplete documentation. Even a simple typo in the claim form can lead to it being rejected. On average, it’s said that 5-10% of all medical claims are rejected because of these small, preventable errors.
Make sure all patient details are correct and double-check coding before submitting the claim. Automation tools can also help in reducing errors by cross-referencing information. Plus, regular training for billing staff goes a long way in avoiding common mistakes. It’s estimated that proper training and checks can reduce rejected claims by up to 25%, which directly translates to smoother revenue cycles.
The Role of Outsourcing in Achieving Clean Claims
Outsourcing billing services takes a lot of the guesswork out of the process. A dedicated team ensures that every claim is accurate, properly coded, and submitted on time. Billing experts stay up-to-date with all the changes in healthcare regulations, so they know how to avoid the common mistakes that lead to claim denials. Outsourcing makes sure that experts handle the tricky process of claim submissions, reducing the chances of errors and increasing the likelihood of submitting clean claims every time.
Studies have shown that outsourced billing services can boost the clean claim rate by as much as 15%, speeding up payments and minimizing rejections. Plus, when claims are processed externally, there’s a built-in system for quality checks before submission, which means fewer rejected claims and quicker payments.
Final Words
Last but not least, getting clean claims isn’t just about accuracy—it’s about efficiency, too. Healthcare providers that focus on submitting clean claims see faster payments, fewer denials, and better overall cash flow. But doing it all in-house can be time-consuming and costly. That’s where outsourcing comes in.
And one of the prominent names in it is Medmax Technologies that has helped healthcare providers recover millions of dollars by streamlining their billing processes and ensuring that clean claims are submitted consistently. So, if you’re looking for ways to improve your clean claim rate and avoid the headache of claim rejections, outsourcing to Medmax Technologies is the smart choice.

Emily Thompson
Emily Thompson is a Revenue Cycle Management (RCM) Specialist with extensive experience in the medical billing industry. She helps healthcare organizations and medical billing companies improve claim efficiency, reduce A/R backlogs, and implement data-driven RCM strategies. Emily’s articles focus on end-to-end medical billing services, denial prevention, and technology-driven revenue optimization for healthcare practices across the U.S.