How are Modifier 91, 59, 25 and 27 Used in Medical Billing
Amid the whirlwind of healthcare operations, accurate medical billing is like the secret sauce that keeps everything running smoothly. It’s not just about making sure the bills get paid; it’s also about ensuring that patients receive the care they need without unnecessary financial burden.
Now, let’s talk about a little something called modifiers. These are like the special ingredients in a recipe that make sure each medical procedure is billed just right. They help paint a clearer picture of the services provided, ensuring fair reimbursement and proper documentation. But today, we’re going to shine a spotlight on one particular modifier: Modifier 91. It’s like the superhero of medical billing, swooping in to save the day when lab tests or procedures need to be repeated.
Understanding Modifier 91
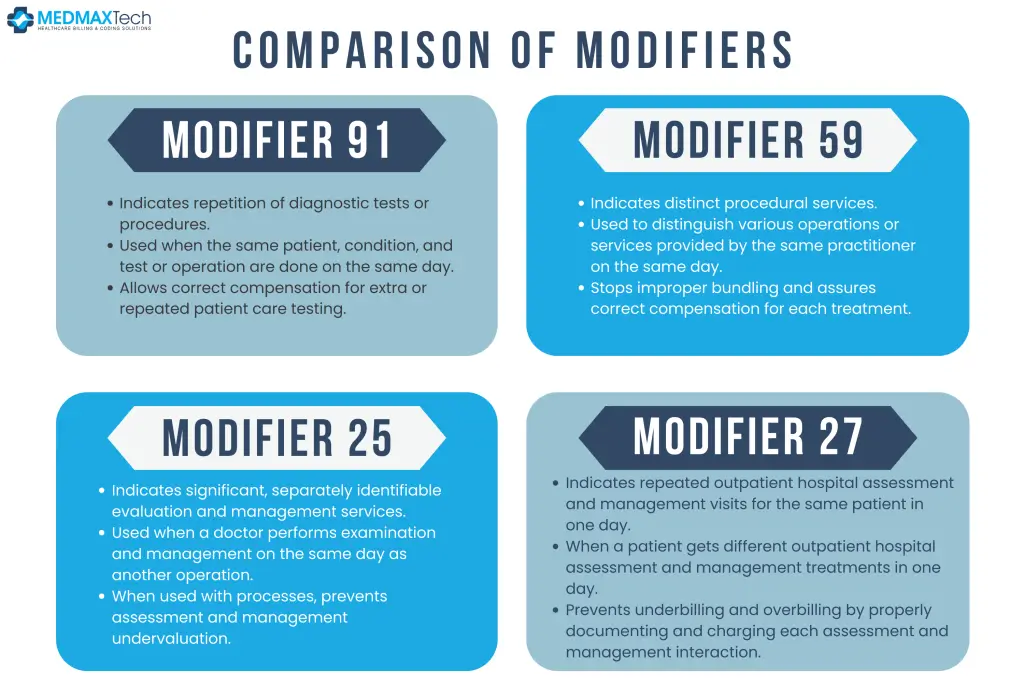
Modifier 91 is a special code used in medical billing services to indicate when a laboratory test or diagnostic procedure has been repeated on the same day. Its purpose is to ensure accurate reimbursement for additional or repeated tests that are necessary for patient care. This modifier tells insurance companies that the repeated test was not just a duplication of the original service, but rather a separate and distinct procedure, which is crucial for AR recovery.
When to Use Modifier 91 in Medical Billing
- Modifier 91 is used when the same laboratory test or procedure is performed on the same patient, on the same day, for the same condition.
- It’s crucial to use Modifier 91 when the test is repeated to monitor a patient’s response to treatment, assess changes in their condition, or confirm the accuracy of previous results.
- This modifier helps healthcare providers avoid billing errors and ensures fair reimbursement for the additional tests performed.
When Not to Use Modifier 91 in Medical Billing
- If you have to repeat a test to make sure the results are correct because the first one didn’t work or the sample wasn’t good enough, don’t use modifier 91.
- If you redo a test to get a different answer, like an extra drug level, do not use modifier 91.
- If you have to take a test again as part of a screening program, do not use marker 91.
Examples Illustrating the Application of Modifier 91
- A patient with diabetes undergoes blood glucose testing in the morning, and the results indicate a need for further monitoring later in the day. When the test is repeated in the afternoon to assess the effectiveness of insulin therapy, Modifier 91 will be appended to the second test.
- A patient presents with symptoms of a urinary tract infection and undergoes a urinalysis in the morning. Later in the day, the physician orders a repeat urinalysis to confirm the diagnosis. Modifier 91 would be used to distinguish the second test from the initial one.
- A patient undergoes a series of blood tests to monitor their response to chemotherapy. Throughout the day, several tests are repeated to track changes in their blood cell counts. Modifier 91 is applied to each repeated test to indicate its necessity for ongoing patient care.
Common Misconceptions About Modifier 91
- Modifier 91 is only used for laboratory tests. – In reality, Modifier 91 can be applied to any diagnostic procedure or service that is repeated on the same day for the same patient and condition.
- Using Modifier 91 will always result in higher reimbursement. – While Modifier 91 ensures accurate reimbursement for repeated tests, it does not guarantee increased payment. Reimbursement rates vary depending on the payer and specific circumstances.
- Modifier 91 is only used for urgent or emergent situations. – While Modifier 91 can certainly be used in urgent cases, it is also applicable in non-urgent scenarios where repeated testing is necessary for proper patient management.
Modifier 59 : Description and Significance
Modifier 59 is a widely used modifier in medical billing solutions that indicates a distinct procedural service. Its purpose is to identify procedures or services that are separate and distinct from other services performed on the same day by the same provider.
How Modifier 59 Differs from Modifier 91
Unlike Modifier 91, which specifically indicates the repetition of a diagnostic test or procedure, Modifier 59 is used to indicate separate and distinct services. While Modifier 91 focuses on repeated tests, Modifier 59 addresses situations where multiple procedures are performed during the same encounter, but each service is unique.
Example of Modifier 59
Modifier 59 is commonly used in situations where multiple procedures are performed in different anatomical sites, different sessions or encounters, different procedures or surgery, or on different organs or structures.

Modifier 27 : Description and Significance
Modifier 27 is used to indicate multiple outpatient hospital evaluations and management encounters on the same day for the same patient. It signifies that the patient received distinct and separate evaluation and management services during a single day.
How Modifier 27 Differs from Modifier 91
While Modifier 27 addresses multiple evaluation and management encounters, Modifier 59 and Modifier 91 focus on distinguishing distinct procedural services and repeated diagnostic tests, respectively.
Example Modifier 27
Modifier 27 is applicable when a patient undergoes multiple evaluation and management encounters in an outpatient hospital setting, such as separate visits to different departments or specialties, each requiring its own documentation and billing.
Modifier 25 : Description and Significance
Modifier 25 is used to indicate significant, separately identifiable evaluation and management services provided by the same physician on the same day as another procedure or service. It helps prevent the undervaluation of evaluation and management services when performed on the same day as a procedure.
How Modifier 25 Differs from Modifier 91
While Modifier 91 specifically addresses the repetition of diagnostic tests or procedures, Modifier 25 focuses on identifying evaluation and management services that are separate and distinct from other procedures performed on the same day.
Example of Modifier 25
A patient visiting their physician for a separate issue during which a procedure is also performed, or a patient receiving an evaluation and management service before a minor surgical procedure on the same day. These scenarios demonstrate the necessity of distinguishing between the evaluation and management service and the procedure itself for accurate billing and reimbursement.
Regulatory Updates and Future Trends
Recent Changes in Modifier Guidelines
In the field of medical billing and medical coding, staying abreast of regulatory updates is paramount. Recent changes in modifier guidelines, encompassing Modifier 91, 59, and 27, among others, necessitate close attention to ensure adherence to evolving coding standards. Regulatory bodies such as the Centers for Medicare & Medicaid Services (CMS) and the American Medical Association (AMA) frequently issue revisions and additions to coding guidelines, reflecting advancements in healthcare practices and technology. By keeping a finger on the pulse of these changes, healthcare providers can mitigate the risk of billing errors and ensure compliance with coding regulations.
Anticipated Developments in Medical Billing and Coding
Looking ahead, anticipation of developments in medical billing and coding is crucial for effective practice management. Emerging trends, including the adoption of artificial intelligence-driven coding software, promise to revolutionize coding processes, enhancing accuracy and efficiency. Moreover, changes in AR Recovery policies and healthcare legislation may significantly impact medical billing practices. Healthcare professionals must remain vigilant, continuously monitoring industry trends and regulatory updates to adapt their billing strategies accordingly.
Potential Impact on Modifier Usage and Reimbursement
The potential impact of regulatory changes and future trends on modifier usage and reimbursement cannot be overstated. As coding guidelines evolve, the utilization of modifiers such as Modifiers 91, 59, and 27 may undergo shifts in application and interpretation. Providers must assess how these changes may affect their billing practices and revenue cycle management strategies. Furthermore, fluctuations in reimbursement rates necessitate proactive measures to optimize modifier usage and ensure accurate reimbursement for services rendered.

Jessica Collins
Jessica Collins is a Certified Professional Coder (CPC) specializing in medical billing services and revenue cycle management (RCM). She works closely with healthcare providers and medical billing companies to streamline claim processing, reduce denials, and enhance reimbursement efficiency.





