How Mental Health Counselling Differ From Hospital Billing?
Mental health counselling billing and medical billing are very one-of-a-kind processes, with mental health billing normally being extra complicated and challenging than medical billing.
The kinds of billing have key regions of variations. As noted above, the nature, complexity, and variability of mental health offerings result in demanding situations with receiving a charge for mental health care.
With mental fitness visits being 5 times extra likely to be out of network than number one or distinctiveness care, it’s vital to recognize those variations for a robust mental health billing process.
Mental Health Counselling Pre-Authorization
Payers commonly have a pre-authorization requirement. Mental health counseling billing services are regularly required to be pre-authorized in advance of time, earlier than the claims are filed.
Mental fitness billing will become greater tough due to the fact oftentimes, gaining pre-authorization is not likely with intellectual fitness claims.
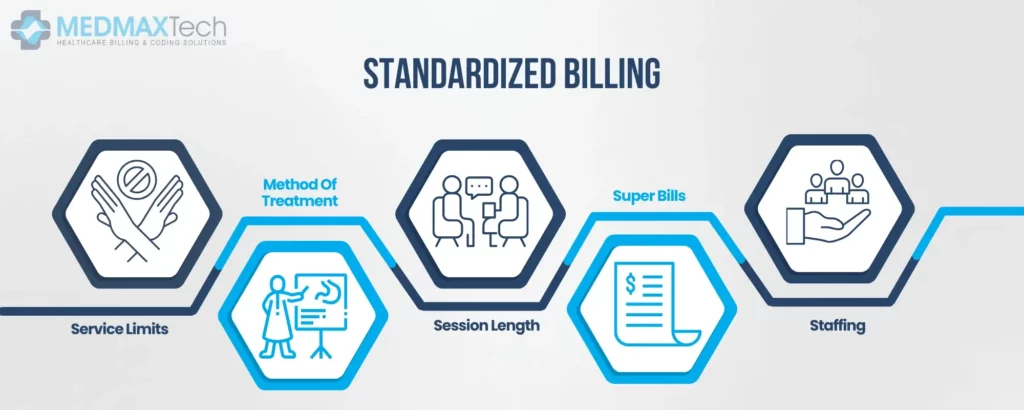
Standardized Billing
Healthcare experts regularly have similar tests, exams, and processes that they run on their patients. There are regularly repeated services, with greater regular and repetitive medical billing. Mental health experts then again offer numerous and specific offerings, growing a more complex billing process.
Overall, this results in much less standardization in mental health billing than with medical billing.
Standardization demanding situations in mental health billing include:
Service Limits
With medical practices, there aren’t generally limits on the frequency of affected person visits. However, for intellectual fitness vendors, insurers regularly enforce a remedy day by day or weekly maximum. These provider limits create intellectual fitness billing complexity.
Method Of Treatment
There are various CPT codes for the healing approach that is utilized by the provider. For example, psychoanalysis has extraordinary coding to behavioral therapy. The excessive variance in coding and breadth of treatments to be had requires an excessive level of expertise.
Session Length
Billing companies for mental health regularly have comparable timings for the length of classes. Medical billing, as a result, regularly operates with this assumption. However, with mental health providers, classes have extremely good variance. Coding for mental health billing is then impacted based on the period of classes with providers.
Superbills
The standardization of medical health practices results in the opportunity for superbills in medical health billing. With those standardized processes, offerings can sincerely be combined into superbills.
Mental health billing services regularly aren’t well matched with superbills because of the dynamic nature of mental health practices. Without superbills, mental health billing is commonly a longer, greater complicated billing process.
Staffing
Medical vendors commonly have a front-workplace staff that manages the medical billing and coding. With this setup, medical practitioners can hold their attention to caring for patients. Mental health practices regularly don’t have this handy setup.
Many mental health vendors are both small partnerships or sole proprietorships and don’t have workers for front-workplace employees. With this staffing distinction and without a dedicated worker to focus exclusively on mental health billing, mental health practitioners regularly manage each affected person’s care and billing themselves.
How To Bill For Mental Health Counseling Billing Services?
Billing for mental health is challenging – however, there are techniques to enhance your revenue cycle management and maximize revenue.
Collect And Confirm Patient Information
Incorrect patient records lead to denied claims and reduced revenue, in addition to time wasted solving errors.
Proactively confirming patient statistics at the start of every appointment guarantees that your exercise has all of the vital records to send bills, request payments, and share communications.
The following records need to be accumulated from a patient’s first appointment, and shown in all next appointments:
- Name
- Address
- Phone number
- Email address
- Insurance records
- Insurance records
- Emergency Contact
- Photo ID
Continuing to confirm this record maintains you up to date on any adjustments in patients’ lives, which includes a move, marriage, or insurance alternate.
Confirm Benefits And Insurance Eligibility
Anytime an exercise takes on a new patient, earlier than the remedy starts it’s critical to understand the whole thing about the affected person’s insurance and price options. Determining what’s covered, what isn’t, and what boundaries exist for the patient’s fee plan is essential.
The key to confirming coverage eligibility and gauging the total image of a patient’s advantages is to accumulate all of the records important to decide a game plan for a way the patient’s care can be paid for.
There are principal matters to search for while confirming insurance:
- An active coverage with correct insurance records
- Benefits included withinside the policy
Create A Telemedicine Billing Plan
As a result of the COVID-19 pandemic, telehealth has exploded for mental health billing services, and this trajectory is expected to continue, with the telemedicine marketplace expected to hit $324.38 billion by 2030.
KFF Data indicates the prominence of telehealth with mental fitness and substance use disorder visits.
Insurance rules to support telemedicine were often evolving with this increased popularity. With increasing services being to be had through telehealth, insurer guidelines and regulations alternate to best accommodate each patient and company’s desires with their policies.
With those constant adjustments in telehealth and its coverage policies, practices need to preserve on top of those policy updates to support today’s needs.
Learn Mental Health Counseling Billing Services Codes
Mental health billing has its very own set of billing codes with CPT. These codes are used for billing and coding in insurance claims, and there are numerous particular codes that mental health practitioners need to use to well identify the services provided.
Learning those codes and how to use them is essential to getting claims paid by mental health companies.
Common mental health CPT codes include:
- 90832 – Psychotherapy, 30 mins
- 90834 – Psychotherapy, 45 mins
- 90846 – Family or couples psychotherapy, with an affected person
- 90847 – Family or couples psychotherapy, with the affected person
Effectively Manage Denied Claims
In 2021, MGMAobserved that 69% of healthcare leaders noticed a growth in denials. Preventing and dealing with denials creates a more healthy revenue cycle control for intellectual health practices.
Creating a plan for easy claims and denial control relieves the stress of denials, and brings extra sales into practice. Ideally, only easy claims are submitted, however, denied claims are inevitable.
Our top denial discount guidelines include:
- Determine the most common reasons for denials for your practice, and cope with the basic causes
- Determine prior authorization
- Quality takes a look at every single claim previous to submission
- Ensure all dedicated staff are knowledgeable and skilled in billing processes
- Follow up with constant denial submissions

Jessica Collins
Jessica Collins is a Certified Professional Coder (CPC) specializing in medical billing services and revenue cycle management (RCM). She works closely with healthcare providers and medical billing companies to streamline claim processing, reduce denials, and enhance reimbursement efficiency.