Medical Insurance Credentialing Guide
Medical insurance company credentialing includes many events and shifting components. Your medical doctor and different healthcare companies all want to show they have the education, training, and competencies required to take care of patients well.
At the equal time, healthcare oversight corporations monitor the work of clinical companies to evaluate, among different matters, reviews of improper care. All of this reporting and tracking need to be usually checked by healthcare facilities that appoint companies and medical health insurance companies that want to issue approved company lists. Indeed, the healthcare company credentialing procedure requires considerable work.
To assist clear the confusion, this article details the fundamentals of company credentialing and gives tips on fulfilling the responsibilities as effectively and efficiently as possible.
What Is Medical Insurance Credentialing In Healthcare?
Provider credentialing in healthcare is the procedure through which clinical corporations affirm the credentials of healthcare companies to make sure they have the required licenses, certifications, and competencies to take care of patients well.
The procedure is likewise referred to as physician credentialing, clinical credentialing, or medical doctor credentialing. Healthcare credentialing is most usually related to the process of authorized physicians. However, even though sometimes less extensive, similar systems are in the area for nurses and different healthcare companies.
The Importance Of Credentialing
Before we begin discussing the steps, let’s answer why credentialing is essential in healthcare to get on the same specific page about the significance of healthcare credentialing, also referred to as insurance credentialing. Most facilities want to ensure their healthcare companies have the proper credentials to process insurance claims. Even if many of your customers are uninsured or pay out-of-pocket, credentialing is vital for providing broad access to care.
There are precise medical doctor credentialing procedures for specific healthcare companies. While the process is essential for physicians, credentialing is likewise vital for Hospitals and fitness agencies, Dentists, Therapists, Licensed massage therapists, counselors, and psychologists.
To be given Medicare and Medicaid, you’ll want to make sure your credentialing branch meets guidelines from the following federal agencies given below:
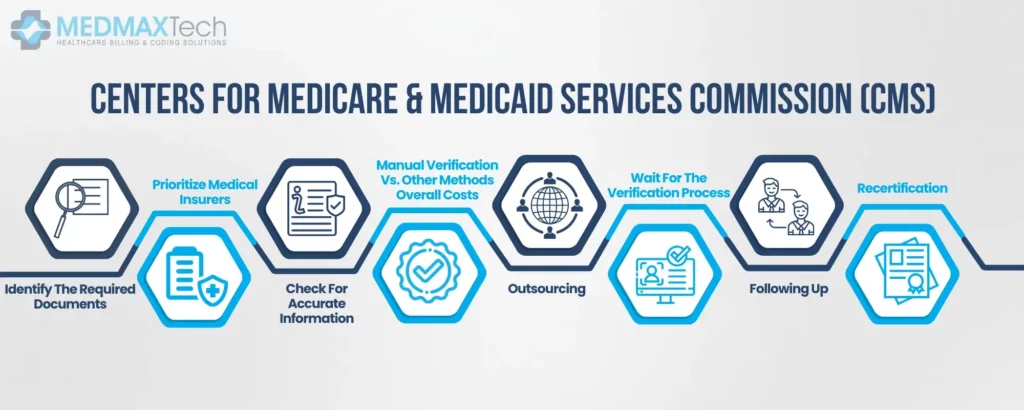
Centers For Medicare & Medicaid Services Commission (CMS)
The Joint Commission of Healthcare Organizations Beyond those federal regulations, every state has its credentialing necessities. Understanding and closely following those requirements can assist reduce your practice’s liability in the face of potential malpractice claims.
As we noted, credentialing is time-consuming or even tedious. Follow those steps to ensure your clinical company gets the proper credentials quickly.
1. Identify The Required Documents
As you start the credentialing procedure in healthcare, ensure that every insurer calls for specific documentation and forms. You’ll want to put up entire applications to every insurer you intend to work with—or even a single missing piece of fact can put off approval by weeks or months.
Make sure your packages are complete and list all insurance companies you intend to file with. Then, list out any required files. These often include but aren’t restrained to:
- Name Social protection number Demographic facts (ethnicity, gender, citizenship, languages spoken).
- Education and residency facts
- Proof of licensure Career record Specialties, and affected person focus Claim records
- Proof of coverage Information about your healthcare facility
Hopefully, tons of those facts were reported for your company’s resume and application. However, you’ll want to take steps to make sure it’s accurate.
2. Prioritize Medical Insurers
Because you’ll want to put up more than one application, it could be advantageous to prioritize which dossiers you put up first. If a considerable part of your clinical billing goes through a single insurer, complete their credentialing application first.
Stay familiar with individual insurers’ regulations. Some insurance corporations—for example, Aetna—permit a streamlined procedure for companies already insured in some other state. That might also additionally imply faster approvals.
Other insurers offer an abbreviated application for companies that are already credentialed in-state. Make a listing of your priorities and start to collect documents and packages accordingly.
3. Check For Accurate Information
As you collect required documents and start individual applications, keep in mind that the quality and accuracy of facts are essential. Before applying, take the subsequent steps: Conduct a background check.
Verify instructional records, licensing, board certification, and recognition through healthcare employers. Any mistakes within the submitted facts can cause trouble. For example, if months and employment dates aren’t quickly and accurately proven by beyond employers, revising the application with the precise information can put off the approval procedure.
Likewise, wrong phone numbers for references or past employers can create delays or rejections. Omissions of past malpractice claims will be disqualifying. Once you’ve assembled and proven those documents, you’re geared to offer them to facility leadership, who will decide the unique privileges to grant to the brand new company. This fact is essential for the credentialing application.
4. Manual Verification Vs. Other Methods
Should your facility manually affirm company facts or use an alternate method?
Some healthcare facilities choose to credential the old school way, calling and emailing medical schools, the American Medical Association, and different vital corporations to verify the facts on a provider’s resume. However, this may be notably time-consuming, and any cut corners could bring about additional delays. Other alternatives consist of: Credentialing software – Programs like Modio and Ready Doc automate components of the credentialing procedure by cross-referencing resume and application facts with AMA profiles, medical schools, the OIG, and more significantly.
5. Outsourcing
Is your HR department overwhelmed with credentialing?
Outsourcing and using a credentialing carrier can potentially keep valuable time and money. Once you’re confident you have the correct information, you could continue to the subsequent step.
6. Wait For The Verification Process
Once you have assembled and submitted your application to insurers, it’s time to look ahead to their approval. This may be a lengthy procedure. While most credentialing may be finished within ninety days, professionals recommend giving yourself one hundred fifty days. If severe troubles arise, credentialing can take even longer.
7. Following Up
Don’t simply wait five or six months to hear from an insurer. Credentialing healthcare specialists reveal that regular follow-ups are essential to timely approval.
Cultivate relationships with key personnel in the insurance company. Established rapport with leadership, executive assistants, and other staff can assist make sure that packages move alongside in a timely way—Check in through the phone rather than email to maximize the risk of response. If you discover that more facts are required, collect and verify all documents in a timely way.
8. Recertification
Eventually, your company will acquire its insurance panel credentialing. However, that doesn’t imply they’ll be credentialed forever. Unfortunately, credentialing is an ongoing procedure that calls for more excellent work down the line.
If you find a mistake in an employee’s facts, it’s vital to inform insurers. If the word is misguided points earlier than you put up a formal correction, it can be grounds for revocation. Most companies want re-credentialing every three years. As we’ve noted, credentialing software programs assist you in controlling credentialing.
Likewise, it must notify you when it’s time to renew a selected company’s credentials. However, insurers have to send a notification after three years have elapsed. Respond in a timely way to ensure your company can offer patient care without interruption.