Ways To Decrease Your Claims Denial
What is claims denial submission? How can you decrease it? Claims denial submission occurs when a claim is submitted by the healthcare provider for an award (to pay for services provided to a patient) and is denied by the payer. Conversely, a rejection occurs when a request is submitted to a payer with incorrect or missing data or coding.
The economy’s state now, with rising unemployment and the closure of many businesses as a result of the global covid 19 pandemic, is putting financial pressure on many people. Even claim submission of healthcare practices aren’t immune to pandemic-related declines. So, in the face of more and more denied claim submission in medical billing applications, it makes sense to make an effort to reduce the number in the interest of the financial strength of your organization.
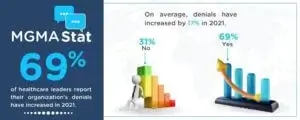
After all, about 69% of healthcare leaders told the Medical Group Management Association that they saw an increase in waste in 2021. For leaders who reported an increase in waste, at least half said it had increased to 10%, with 12% saying the increase was 30%. These statistics would give any medical service provider pause, prompting a search for a solution.
You are tackling the rampant volume of denied complaints benefits practices of all sizes, from family physicians to large multi-specialty groups. Reduce your claims denial rate with these seven steps.
How To Decrease Claims Denial Submission In Medical Billing?
1. Verifying Patient Information In Advance:
Some medical organizations are so busy or under-staffed that they don’t take the time to verify crucial details of the patients they diagnose and treat. However, this can be a recipe for financial disaster. It should be emphasized why it is essential to reduce the refusal of complaints. Some 42% of health care professionals told the MGMA that prior authorization was why they saw denials.
Train your team of professionals to collect this vital information as soon as possible, such as when you make an appointment or when the patient presents. Software tools can help you automate this process, saving you time by requiring staff to manually call each request to providers to verify each patient’s insurance status. In any case, you take care of this task. It would be best if you did this regularly in the future.
2. Remind Patients Of Their Responsibilities:
A problem may be not communicating the details of what your patients are responsible for. A sign at reception is an excellent place to start. You can also include a standard form for patients to sign, acknowledging that they have been informed of their payment responsibilities.
Other ways to convey this information forward include posting the news on your websites and having it in a newsletter article that you regularly email to patients.
3. Updating Training/Staff Integration:
Sometimes cracks occur in an organization due to inconsistent (or insufficient) staff training professionals. Start this by meeting with your staff to reiterate that they must provide all necessary clinical documentation or evidence to support the diagnoses and treatments you offer. Adjustments to care should be noted and justified, such as giving codes to explain extended stays for patients or a particular treatment modality.
Prioritize staff who become more accurate in medical coding. They may need the training to get up to speed. All of these concerns should also apply to the process of recruiting, hiring, and onboarding employees.
4. Submit Complaints In A Timely Manner:
MGMA research indicates that 7% of healthcare professionals surveyed found “timely reporting” issues to be the reason for denied complaints. This is anything that any medical team can quickly fix. Send them according to schedule. Identify why some of them are late.
Was it an oversight?
Are your staff so overworked that they are unable to complete documentation and complaint requirements on time?
Discover the primary sources of delays to optimize the responsiveness of your organization.
5. Update Your Computer Systems:
Your computer system has probably not been updated for some time. Medical practices prioritize risk avoidance, and changing computer networks and installing the latest version of the operating system and essential software can worry those responsible for downtime. But a modernized IT setup allows your staff to work faster and more efficiently. It also gives you the latest security protection and lets you distribute specialized software to handle claims denial.
6. Use Software Designed To Handle:
Denied Claims submission? Don’t try to get away with using a generic computer application to organize and process claims for submission to insurers. Use a comprehensive Denied Claims Management software solution. Your team all denied claims along with the reason for non-payment. Then you use the software to make the necessary corrections and resubmit your claim on the spot.
7. Prioritize Reducing The Number Of Denied Complaints:
Focusing on reducing the percentage of denied complaints will make a real difference to your organization’s revenue stream.
Fewer denied claims could allow for budget flexibility, devote additional resources to staffing, or invest in equipment upgrades to further benefit the practice and the patients you care for.
Key Points:
- With people under financial pressure, it is more important than ever for medical organizations to reduce the number of denied claims.
- At least 69% of health officials report an increase in denied claims in 2021.
- Ensure your staff check patients’ insurance status before diagnosing and treating them.
- Remind patients of their financial responsibilities to avoid confusion or late payment.
- Retrain staff and improve staff onboarding as needed to correct errors that may lead to denied requests.
- Utilize specialized claims denial management software for enhanced efficiency and cash flow improvement.
Final Verdict:
Denying availability claim submission puts a heavy strain on healthcare worker budgets, which many organizations cannot afford today, given the current pandemic. In an environment where everyone has to do more with less, reducing claim denials could free up vital income and staff time to create room for quality improvement.
The Good News?
Approximately 90% of claims denial can be avoided when healthcare providers automate revenue cycle functions. In fact, vendors could save around $9.5 billion by automating their claims handling processes.